03 9576 0088
info@simonjakobovits.com.au
Private Practice: Suite 32, Cabrini Medical Centre
Isabella Street, Malvern 3144, Melbourne, VIC, Australia
Gastroscopy | Colonoscopy | Flexible Sigmoidoscopy
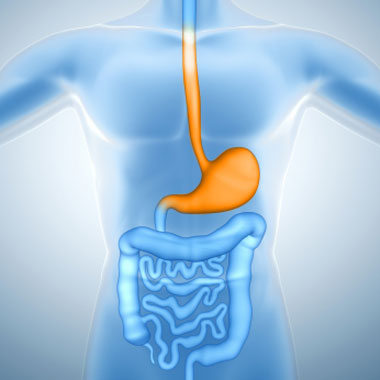
What is a Gastroscopy?
A Gastroscopy is a procedure used to examine the upper digestive tract; including the esophagus, stomach and start of the small intestine. It is performed to investigate symptoms such as swallowing difficulties, upper abdominal pain, heartburn, loss of weight and anaemia.
After a fast of several hours, the patient is sedated (made sleepy) by a qualified anaesthetist who injects a sedative via a cannula (tiny hollow plastic tube) inserted into a vein. This is not a general anaesthetic but the patient is asleep.
When the patient is asleep a flexible tube about 70cm long and about 9mm in diameter is passed through the mouth and down the esophagus, passing through the stomach and ultimately reaching the duodenum (start of the small intestine). Throughout the procedure images of the lining of the upper digestive tract are seen in real time on a television screen.
Lesions such as ulcers, polyps, cancers, inflamed areas and abnormal veins, among other things, can be seen. If necessary, lesions can be sampled by taking a biopsy (a small “pinch” of tissue) to be sent to the lab and examined under a microscope. Some lesions can be completely removed with a snare (a wire loop). It is also possible to undertake procedures to stop bleeding lesions such as ulcers and abnormal blood vessels.
A standard diagnostic gastroscopy (examining to find a cause for symptoms) takes about 10 minutes and is very safe. After the procedure the anaesthetic drug wears off very quickly and you are given something to eat and drink. Dr Jakobovits will then review you before you go home and inform you of the examination findings and the follow up plan.
Some therapeutic gastroscopies (procedures undertaken to treat a problem such as dilating a narrowed esophagus or stopping a bleeding ulcer) take longer and Dr Jakobovits will speak with you specifically about these procedures prior to the gastroscopy should he feel they are likely to be required.
What do I need to do to prepare for a Gastroscopy?
• You are to fast (nothing to eat or drink) for 6 hours prior to your arrival time.
• Please don’t bring any valuables with you. Wear light clothing as you will be required to change.
• Bring your private insurance and medicare details with you.
What happens on the day of the procedure?
• Please arrive at the Day Procedure Centre at Cabrini Hospital Malvern at the designated time.
• Feel free to bring something to read/do as your arrival time is not the procedure time. You need to check in and change into a hospital gown, which can take some time. In addition the time taken for the cases ahead of you can vary depending on complexity so the exact procedure time is unpredictable. Whilst our best intentions are for you to not wait too long, each procedure is unique and sometimes a person on the list in front of you will have an unexpected finding which may prolong their procedure time and your wait. You can expect to be at Cabrini for approximately 4 hours from arrival time to departure. Sometimes this is much faster and we can call your “pick up” person when you are ready to go.
• Once in the examination room, the anaesthetist will administer a sedative agent to make you sleepy and comfortable. It is not a general anaesthetic, but almost all patients are unconscious and have no recollection of the procedure. Occasionally some patients momentarily rouse and may have some recollection of the event. It is not generally painful.
• The time taken to complete the procedure varies, but is generally around 5-10 minutes.
• Depending on the findings, biopsies (samples) may need to be taken, or polyps (small growths of the bowel lining) may be removed.
What happens after the Gastroscopy?
• After the procedure you will be taken to the Recovery Area until any sedation wears off – it’s not uncommon to have some bloating after the procedure or a sore throat. These will both pass over a short time.
• When you are awake, Dr Jakobovits will review you and explain the results of the examination to you. Follow-up arrangements will be made.
• You will be given discharge instructions
• After you have had something to eat and drink you will be able to go home – You are not allowed to drive home, or drive or operate dangerous machinery for the rest of the day/night. Do not sign any legal documents or drink alcohol during that same period of time.
• If you cannot find someone to pick you up after your procedure, you can go home in a taxi, but we will keep you for longer to make sure you are alright and it is our preference that a responsible adult be with you for the remainder of the day.
• On the morning of the following day you can resume all normal activities.
Safety and risks
• All activities carry some risk including driving a car. Medical procedures are no different, however Gastroscopy is a very low risk procedure.
• It is not uncommon to have a mild sore throat after a gastroscopy. It generally only lasts a day or so and usually requires no specific treatment. Bloating can be experienced as air is pumped into the digestive tract to open it up and allow adequate inspection of the lining. This is usually minor and passes very quickly.
• Aspiration is the passage of saliva or gastric contents into the lungs whilst a patient is asleep. This can result in irritation or infection of the lung (pneumonitis/pneumonia). The most likely reason for this is not fasting for long enough prior to the procedure. It is not common and can usually be treated with antibiotics and rarely requires admission to hospital for observation and treatment. It is important to follow the preparative instructions carefully.
• Bleeding can rarely occur and is almost always treatable through the ‘scope. Some procedures such as removing polyps and dilating narrowings increase the risk of bleeding. Taking medicines that thin the blood such as Plavix and Warfarin also increase the risk of bleeding.
• Infections following a gastroscopy are exceedingly rare due to the strict cleaning procedures undertaken on the equipment after each procedure.
• Perforation (making a hole in the digestive tract) during a gastroscopy is rare (1/10,000).
• While gastroscopy is the most accurate means of assessing the bowel, it is possible to miss small but important lesions.
Gastroscopy | Colonoscopy | Flexible Sigmoidoscopy